WHAT ARE THEY?A varicose vein is a dilated vein that is clearly visible on the skin or palpable under the skin. Varicose veins are usually blue and winding, and are mainly found on the legs. Varicose veins are very common and are among the top ten complaints for which people visit their doctor. They are more common in women than in men. The medical term for varicose veins is varicose veins.
Varicose veins come in all shapes and sizes:
 |
 |
 |
 |
| Small varicose veins (spider veins) |
Large varicose veins (large side branches) |
 |
 |
| Large varicose veins (main veins) |
WHAT IS THE FUNCTION OF VEINS?Veins are the blood vessels that ensure the return of blood to the heart. The arteries carry blood from the heart to the legs, and then it flows back to the heart via the veins. On the outside of the leg, there's a network of superficial veins through which the blood flows upward. Inside the leg, between the muscles, there are also large veins through which the blood flows. All these veins contain valves. These valves ensure that the blood can flow smoothly from the toes back to the heart. When you walk or move your leg muscles, the veins are squeezed empty, and because of the valves, the blood can only flow in one direction—up.
If the valves no longer function properly or are damaged, blood flows less easily back to the heart. This causes the vessels to become congested, widening, congested, and tortuous: this is how varicose veins develop.
WHERE IN THE LEG ARE THE VEINS?The venous system of the legs consists of the superficial and deep systems. The superficial system consists of numerous small veins that enclose the leg like a net. Approximately 10% to 20% of the blood from the superficial veins collects in the large main veins (the so-called great saphenous vein (VSM) and the small saphenous vein (VSP)). These two main veins empty into the deep system at the groin and popliteal fossa, respectively. Blood is also transported from the superficial to the deep system via connecting veins (perforating veins). This deep system provides the majority (90%) of the blood flow from the legs and is invisibly embedded in the leg muscles.
The veins in the leg. The light blue vessels are the deep system, the dark blue vessels are the superficial system. In the patient on the left in the image, all the valves that should have been in the main vein of the femur have ruptured. This has created a massive varicose vein.
WHAT CAUSES VARICOSE VEINS?Varicose veins usually develop because the valves in the veins no longer close properly. As the veins widen over time, the valves close less effectively. The valves can also be damaged by a previous thrombosis. If the valves no longer function properly, the blood doesn't flow back to the heart properly, and the pressure in the vein increases. This causes the vein to expand. This expansion also prevents the valves further down the line from closing properly, furthering the process.
Varicose
veins tend to run in families. Hereditary factors therefore play a role. Sometimes there is a congenital weakness of the supportive tissue around the veins, which can lead to varicose veins. Sometimes the valves in the veins are not properly formed or are missing altogether.
Hormonal factors
: The fact that women suffer more frequently from varicose veins is attributed to the influence of female hormones, but also to the use of the contraceptive pill, and previous pregnancies.
Pregnancy:
During pregnancy, the connective tissue everywhere weakens under the influence of pregnancy hormones, making it easier for veins to expand. In addition, the blood vessels become congested because the uterus compresses the duct. These two factors often lead to varicose veins during or after pregnancy.
Standing work:
Varicose veins are more common in people whose jobs require standing (e.g., hairdressers, teachers), especially if they require a lot of lifting (e.g., machinists). Thrombosis in the leg:
Varicose
veins can also be caused by a thrombosis in the leg. With a thrombosis in the leg, deep veins in the leg are usually blocked by clotted blood. This overloads other veins on the outside of the leg, which can lead to varicose veins. The valves in the vessels deep in the leg can also be damaged by thrombosis. The blood clot in the veins is usually completely cleared after a few months, but the valves can be destroyed during this process.
Surgery and accidents:
Veins can also be damaged after surgeries, such as hip and knee replacements, and after accidents.
Obesity:
Varicose veins are more common in people who are overweight.WHAT ARE THE COMPLAINTS AND SIGNS?Varicose veins often cause no symptoms at all. Many people find their presence bothersome or unsightly. Varicose veins usually gradually worsen over the years.
If varicose veins do cause symptoms, they usually present as a tired, lethargic, and heavy feeling in the legs. Sometimes, people experience itching and tingling, difficulty keeping their legs still in bed (restless legs), or a feeling of something crawling on their legs. In rare cases, pain or bleeding from a varicose vein occurs. In addition, poor blood flow back to the heart (venous insufficiency) can also cause congestion and, as a result, fluid retention (edema) around the ankles. These symptoms worsen throughout the day, after standing for long periods, and in warm weather. If fluid retention persists for a long time, symptoms may develop on the lower legs, such as pigmentation, eczema, white scarring, hardening of the skin and subcutaneous fatty tissue and ultimately an open leg (ulcus cruris venosum).HOW IS THE DIAGNOSIS MADE?Varicose veins are easy to recognize, but if larger ones are present, further examination is necessary. Varicose veins on the outside of the leg can be the result of leaky valves deep within the veins. This must first be examined; this examination is usually called phlebodiagnostics . During this examination, the location of the varicose veins, their type, and the best treatment are determined.
The examination for varicose veins is performed while standing, because then they fill and are clearly visible. First, the location of the varicose veins is determined and whether they are large or small. The next step is examining the two large main veins: the great saphenous vein in the groin and the small saphenous vein in the popliteal fossa. Using a duplex device (ultrasound-Doppler), the valves in the veins and the direction of blood flow are examined. The duplex device can also detect clogged vessels (thrombosis) and the functioning of the deep vein system.
 |
 |
| Duplex device |
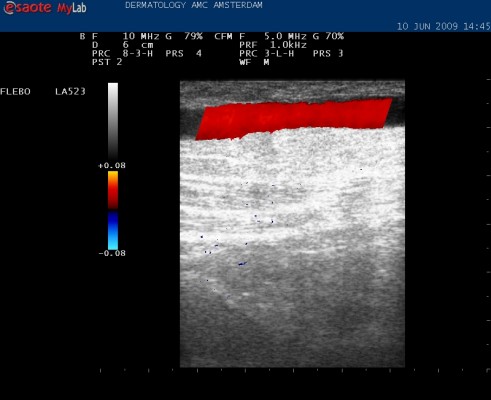
A leaky barrel in the depths: colored red on the Duplex screen |
On the Duplex device's screen, the vessels are visible as black indentations against a grayish-white background. If your calf is squeezed during the examination, the blood will flow upward. This is indicated by a blue color on the screen – this is normal. If the valves are not functioning properly, the blood will flow back down the varicose vein. This is indicated by a red color on the screen – this means the valves are not functioning properly. By examining various areas – the groin folds, the backs of the knees, and elsewhere on your leg – a clear picture of the leak and what needs to be treated
is obtained. You will then receive advice and treatment plans. You will also receive written information to read at home.HOW IS THE BEST TREATMENT DETERMINED?This is determined based on the findings during the examination. If you only have small varicose veins on the outside of your leg, injection ( sclerosis ) is the best solution. If there are very small ones, so small that a needle cannot fit, they can be treated with an external laser treatment. For medium-sized varicose veins, sclerotherapy is also the best solution. For very large varicose veins, sclerotherapy is not the best treatment because it often becomes ineffective: the vessel can reopen later. Furthermore, a large amount of sclerosant must be injected. These varicose veins are best cauterized from within ( endovenous treatment with the VNUS method ). Alternatively, foam sclerotherapy can be used. For very tortuous varicose veins or large varicose veins that lie just beneath the skin, cauterization from within is not effective. In that case, the vascular surgeon can surgically remove (strip) the vessels. The vascular surgeon can also connect the connections to the deep system (perforantectomy). Large side branches of the main veins are best removed through small incisions under local anesthesia. This is called the Muller procedure (outpatient phlebectomy). If the valves in the vessels of the deep system are defective, then treating external varicose veins is not very effective. In that case, you should wear elastic stockings (compression therapy).OVERVIEW OF THE DIFFERENT TREATMENTS FOR VARICOSE VEINSElastic stockings and pressure bandages (compression therapy)
Sometimes it is decided not to treat varicose veins. For example, because the deep vein system is compromised. Or because treatment is not yet possible, for example, during pregnancy or shortly after a deep vein thrombosis. In these cases, wearing elastic stockings can significantly reduce symptoms.
Sclerosing (varicose vein injection)
With sclerosing, the varicose veins are injected with an irritating fluid (ethoxysclerol). This substance causes an inflammatory reaction in the vessel wall. A pressure bandage (compression bandage) or elastic stocking is then placed around the veins, pressing them together. The damaged vessel walls then adhere to each other, and the vessel closes. A variant of sclerosing is foam sclerosing. For this, the sclerosing fluid is mixed with air to create a foam. This foam makes better contact with the vessel wall, allowing larger vessels such as the trigeminal veins to close.
Muller procedure (outpatient phlebectomy)
The Muller procedure is intended for large, superficial side-branch varicose veins. The varicose vein is marked. Under local anesthesia, small incisions are made alongside the vein using injections of anesthetic fluid. The varicose vein is then pulled outward with a hook. The incisions heal very well. To prevent bruising, a pressure bandage is applied for two weeks.
Endovenous techniques (cauterization from within)
This is the newest method for treating large-stem varicose veins (great saphenous vein and small saphenous vein) without surgery. Endovenous means that the vessel is cauterized from within. There are various techniques, including laser, radiofrequency, steam, and freezing. The method is always the same: the vessel is punctured under control with the Duplex device. A small tube is advanced into the vessel, and through this tube, the vessel is damaged from within. Ultimately, the vessel shrinks and becomes completely closed. The latest and best technique is the VNUS closure method . This works with radio waves, the same principle as in a microwave.
Surgery (crossectomy + stripping)
The large saphenous veins (the great saphenous vein and the small saphenous vein) can also be surgically removed. This is performed by a vascular surgeon under general anesthesia or with a spinal injection. This procedure is becoming less and less necessary due to new endovenous techniques. However, it is still performed, as some vessels are not suitable for endovenous techniques, for example, if they are too tortuous or run too close to the skin. During a crossectomy, the entrance of the VSM or VSP into the deep vein system is located through an incision in the groin or popliteal fossa, respectively. The connection of the VSM or VSP to the deep vein is then severed, and all side branches are tied off with sutures.
A crossectomy of the VSM in the groin is often combined with stripping. During stripping, a wire is passed through the main vein from the groin to the knee. The VSM is attached to the end of this wire and then pulled out inside out (stripping).
Can I simply do without these large veins?
Yes. This type of procedure is only performed on veins that no longer function properly: they are too large, the valves are malfunctioning, they are congested, they cause symptoms, and they no longer truly contribute to the return flow of blood. They can even cause problems, such as clots, phlebitis, and fluid retention in the leg and skin changes. You could miss these veins like a toothache. The return flow of blood is taken over by the many other vessels on the outside of the leg and inside the leg.
Combination of surgery, other techniques, and sclerotherapy.
Often, a combination of various techniques is used to achieve the best result. This is done in several stages. The larger varicose veins are addressed first using the described surgical and endovenous methods and foam sclerotherapy. Afterward, the remaining varicose veins can be treated with, for example, sclerotherapy.
Complications of surgery.
Properly performed treatment for varicose veins carries few risks. In some cases, a limited phlebitis can occur. After surgery, blood can leak from a operated vein, causing a bruise (hematoma).
Complications of sclerotherapy
: Sclerosis is usually (> 95%) uneventful, but mild complications can occur, and with very small veins, the effect can be disappointing. It is good to be aware of this beforehand.
When injecting varicose veins, brown discoloration of the skin can occur, especially in people with pigmented skin. Sometimes a test spot is done first to assess whether discoloration occurs. It can take months to a year for the discoloration to disappear, and in less than 1% of cases, it is permanent. The injection of the fluid can cause itching or pain; this is temporary and resolves on its own. Sometimes people are allergic to the fluid and develop hives or other allergic reactions. These can be treated, but further sclerosing is not possible in that case. Bruising can occur. Clots can form in and around the vein, which feel hard, like elongated strands or bumps under the skin. These clots are cleared by the body, just like bruises. If the injection fluid gets next to the blood vessel, the skin at that location can become damaged. Sores or ulcers may develop. When sclerosing very small blood vessels (varicose veins), new, even smaller veins may develop around the veins after injection. This is called telangiectatic matting. It occurs in less than 1% of cases. The cause is unknown. It usually disappears on its own within 3 to 12 months. Furthermore, injection may not be possible for varicose veins with varicose veins because the vessels are smaller than the needles used. Laser treatment for this type of very small varicose veins may be an option. A (too) tight bandage or stocking can cause skin blisters and pain. If pain occurs, the stocking or bandage should be removed and replaced with a looser-fitting stocking or a looser bandage. Thrombosis or pulmonary embolism after varicose vein treatment is rare.IS THE TREATMENT REIMBURSEED?In 2012, health insurers changed their reimbursement rules. Treatment for small varicose veins is no longer covered. You must pay for the treatment yourself, and due to the new DBC (Disability Testing) system, which also includes various hospital costs, it can be very expensive. Very large varicose veins, which also cause symptoms such as fluid retention (edema), are still covered. These include the large main veins and their large side branches. Some hospitals still treat small varicose veins, but no longer charge for them. Other hospitals charge a separate fee for cosmetic procedures. However, a growing number of hospitals are discontinuing the treatment of varicose veins that are only cosmetically relevant; it can still be performed in private clinics.WHAT CAN YOU STILL DO YOURSELF?Walking and exercise are important for good results. It's wise to take a walk every day. Prolonged standing, sitting still, heavy lifting, and heat should be avoided. When sitting for extended periods, it may be wise to elevate your legs.WHAT ARE THE OUTLOOK?Depending on the size and cause of the varicose veins, a particular treatment will be more or less successful. For some, varicose veins return quickly, while for others, they remain absent for several years. What the practitioner is essentially doing is clearing up varicose veins; the treatment does not eliminate the tendency to develop them elsewhere.HOW DO I MAKE AN APPOINTMENT FOR VARICOSE VEIN TREATMENT?There are several hospitals and specialized clinics where you can have varicose veins treated.
In the Amsterdam region, you can go to the Huid Medisch Centrum (Skin Medical Center) .
You will need a referral from your general practitioner. |