WHAT IS A HYDROCOLLOID DRESSING?A hydrocolloid dressing is a self-adhesive bandage a few millimeters thick, usually light brown, that can be applied to a wound and left in place for several days. It is also called a second skin. Hydrocolloid dressings consist of two layers: the top layer is a sealing plastic film (polyurethane film), and the bottom layer is the hydrocolloid. The hydrocolloid material is a mixture of adhesives such as polyisobutylene and pectin, gelling agents (which form a gel) such as gelatin, and absorbent particles such as carboxymethylcellulose. Polyisobutylene is a sticky, rubbery substance. Carboxymethylcellulose is a highly absorbent substance made from plant fibers (wood pulp).
 |
|
 |
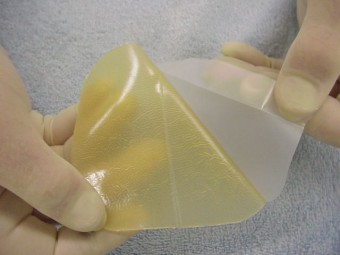
example of a thick hydrocolloid
|
|
hydrocolloid layer and foil
|
 |
|
 |
| DuoDerm E hydrocolloid dressing |
|
Duoderm Extra Thin |
The hydrocolloid layer absorbs wound fluid and liquefies into a gel that makes contact with the wound bed. The amount of wound fluid a hydrocolloid dressing can absorb depends on the thickness of the hydrocolloid layer. There are thick hydrocolloid dressings such as DuoDERM E and thinner ones such as DuoDERM Extrathin. When the dressing is full and leaks, it must be replaced.
DuoDERM is a brand name. Duoderm, manufactured by Convatec, was one of the first hydrocolloid dressings on the market. Many other brands are now available from various suppliers. Some examples of hydrocolloid dressings are Duoderm, Duoderm E, Duderm ExtraThin, Duoderm Signal, Comfeel Plus, Combiderm, Askina Hydro, Kliniderm Hydro, Nu-derm hydrocolloid dressing, Suprasorb H, and Tegaderm hydrocolloid dressing. For more information about the different hydrocolloid dressings (variants, brands, sizes, order numbers and prices): see the product overview .HOW DOES A HYDROCOLLOID BANDAGE WORK?A hydrocolloid dressing is applied over a wound, completely blocking it from oxygen. The bottom layer of the dressing absorbs wound fluid and melts into a gel that makes good contact with the wound bed. Hydrocolloid dressings are particularly effective because they create a moist wound environment. The wound healing process is faster in a moist wound environment than in a dry one. Chronic wounds often contain dead tissue, which must be cleared by immune cells (leukocytes and macrophages). These cells can perform their function better in a moist wound than in a dried-out, crusted wound. Skin cells can also grow back better and faster in a moist wound than in a dry one. Wounds that are kept moist often experience less pain.
In addition, the hydrocolloid layer with the plastic top layer hermetically seals the wound from oxygen. Bacteria that require oxygen to survive (aerobic bacteria) are killed by this. Bacteria that can survive without oxygen (anaerobic bacteria) remain. A hydrocolloid dressing therefore kills some of the bacteria.
Furthermore, there is a theory that sealing a wound from oxygen stimulates the formation of new blood vessels. A difference in oxygen concentration stimulates blood vessels to grow, and they proliferate towards the area where the oxygen concentration is lowest. Hydrocolloid dressings can stimulate the formation of new blood vessels. Red tissue develops in the wound, also called granulation tissue. Granulation tissue fills the wound, and then skin grows over it at the edges.FOR WHICH WOUNDS CAN A HYDROCOLLOID DRESSING BE USED?Hydrocolloids can be used on a wide variety of wounds and in almost all phases of wound healing. They are used for open leg ulcers (venous leg ulcers), pressure ulcers (decubitus ulcers), and numerous other wounds. The thicker hydrocolloids can also be used to protect the skin from pressure. Skaters use them to protect their feet from blisters, and cyclists use them to allow them to continue cycling with abrasions. Another application is the use of hydrocolloids on the intact skin around a wound, protecting it from moisture or the adhesive layers of other dressings.
They are not recommended for deep wounds with extensive slough and undermined wound edges (deep cavities and cracks), as there is a risk that the wound fluid cannot drain.ARE THERE SIDE EFFECTS OF HYDROCOLLOID DRESSINGS?Skin irritation and allergy to the adhesive layerHydrocolloids with an adhesive layer can occasionally irritate the surrounding skin. Contact allergy to the adhesive layer also occurs.Softening of the skin around the woundThe top layer of the skin, the stratum corneum, turns white due to prolonged exposure to moisture. This isn't a major concern; the positive effect of the moist environment on the wound outweighs the slight damage caused by moisture on the surrounding skin.The wound seems to be getting biggerThe dressings soften the wound, remove dead tissue, scabs, and the surrounding skin. Due to the softening effect, a wound may appear slightly larger at the first dressing change. This isn't actually the case; the wound doesn't get any larger. In its dried state, the wound was somewhat more contracted.There's a nasty smelly amount of pus coming out from underneath!When a hydrocolloid dressing is removed after a few days, it's often a bit of a shock to see what emerges from underneath. A foul-smelling, pus-like sludge is released. However, this isn't pus, but a pus-like mixture of the liquefied hydrocolloid material, wound fluid, and remnants of dead tissue. The odor is due to the anaerobic bacteria that survive under an occlusive hydrocolloid dressing, which can emit a sickly, foul odor. It's good to be aware of this beforehand and that it's normal; otherwise, you might think the dressing is making the wound worse. Rinse and/or remove the sludge by dabbing the wound a few times with gauze soaked in saline (0.9%) or water, and the wound will look good again.Wound infectionInfection with harmful bacteria can occur under a hydrocolloid dressing, but this is rare. If there are signs of infection (redness around the wound, swelling, warmth, pain, fever), an antibiotic should be started.Excessive granulation tissue (hypergranulation tissue)Hydrocolloids can stimulate the formation of granulation tissue (newly formed blood vessels), which is the intention of the product, but sometimes it goes too far. Excessive granulation tissue (hypergranulation), which protrudes beyond the wound edges, is also not good. The ingrown skin then has difficulty growing over it. Excessive granulation tissue, also called "protruding flesh," can be addressed with silver nitrate pens or surgically removed. |