| HEMORRHOIDS |
 |
 INTRODUCTION INTRODUCTION
This brochure provides a general overview of the symptoms, causes, and treatment of hemorrhoids.
It is important to realize that when diagnosing a condition, the situation can be different for
everyone.
WHAT ARE HEMORRHOIDS?
Hemorrhoids are swollen blood vessels near the anus. Everyone has these blood vessels. They are
located on the inside at the end of the rectum and the beginning of the sphincter muscle. Such a
swelling is a spongy network of blood vessels, covered by a thin layer of mucous membrane.
Hemorrhoids are therefore actually swollen blood vessels. They can best be compared to varicose
veins. However, they are located in an uncomfortable place: inside the sphincter muscle of the anus.
Sometimes they become so swollen that they protrude outside the anus. This can be painful,
especially during and after bowel movements. Sometimes they bleed or become inflamed. However,
not all bleeding from the anus is caused by hemorrhoids. Even if you are sure you have hemorrhoids,
the bleeding may still be caused by something else. That is why your doctor must always determine
the exact cause of any bleeding.
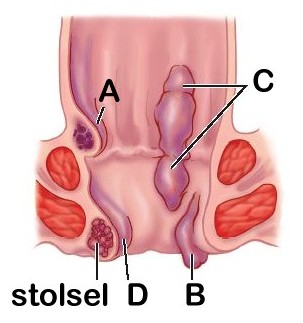
A) Internal hemorrhoids
B) External hemorrhoids
C) Combined internal and external hemorrhoids
D) Thrombosed hemorrhoids (a clot has formed in the
dilated vessels of the hemorrhoid)
WHAT IS THE CAUSE?
In themselves, these swollen blood vessels are nothing more than weak spots. Nothing unusual, in
other words. It only becomes a problem when a lot of pressure is exerted on those areas. And in the
vicinity of the anus, they often have to endure quite a lot. There can be various reasons for this, such
as sitting too much and not getting enough exercise, or being overweight. But the main cause lies in
our diet. Nowadays, food contains less fiber. Fiber is indigestible and retains moisture, making stools
soft and loose. The lack of fiber in our diet therefore results in hard, dry stools. This makes bowel
movements more difficult. We have to strain and push. This puts a lot of strain on those weak areas.
They become irritated and swell up. This can cause hemorrhoids to develop and prolapse.
WHAT SYMPTOMS CAN HEMORRHOIDS CAUSE?
Hemorrhoids can cause various symptoms. Sometimes they prolapse, possibly even through the
sphincter muscle. This usually causes a feeling of fullness. The mucous membrane on the hemorrhoid
can become vulnerable, causing bright red blood to appear on the toilet paper when wiping. It is also
possible that some intestinal mucus and/or loose stools 'leak' through the sphincter muscle. This
often causes annoying itching.
If the hemorrhoids in the anus become pinched, they swell further and there is a chance that they
will rupture. This causes you to lose some bright red blood after or during a bowel movement. The
sphincter muscle of the anus and the skin around this area usually become irritated, resulting in a
burning sensation and itching.
When the constriction increases, pain often occurs. Sometimes a painful swelling also develops in the
anus. The blood flow in the hemorrhoid can stagnate, and a clot (thrombus) can form. Such a blood
clot in a hemorrhoid (thrombosed hemorrhoid) is often very painful.
CAN HEMORRHOIDS BE CURED?
Once hemorrhoids have prolapsed, they remain prolapsed. Certain measures and lifestyle changes
can prevent or alleviate symptoms.
HOW CAN WE PREVENT SYMPTOMS?
Symptoms can be prevented by keeping your stools soft. This requires eating sufficient plant fiber
(bran, brown bread, etc.) and drinking plenty of water. Bran is best. You can buy it at the grocery store
or drugstore. Add a tablespoon to a cup of yogurt. Start with three times a day. Soon your stool will
become less hard and dry. If it becomes too loose, you can reduce the amount to one or two
tablespoons a day. You will know best what is right for you.
Furthermore, when you feel the urge to have a bowel movement, do not delay going to the toilet for
too long. A certain regularity prevents you from having to hold back at inconvenient moments.
Avoiding straining as much as possible also prevents complaints of prolapsed hemorrhoids.
Regular warm baths help the anus to relax. A warm sitz bath is also a good way to combat symptoms
such as burning, pain, itching, and eczema around the anus (hygiene).
Ointments and suppositories can relieve pain and burning.
Make sure you get some more exercise, especially if you lead a sedentary lifestyle. And if you are
overweight, try to lose some weight.
Do not consume too much coffee, tea, carbonated drinks, and sugar. They irritate the anus and can
cause itching and eczema. Hemorrhoids are an annoying condition. But with a little care and
regularity, you can get rid of them.
Most patients with hemorrhoid complaints benefit from these measures and lifestyle rules.
WHEN IS SURGICAL TREATMENT NECESSARY?
If the symptoms persist despite taking the above measures and lifestyle rules, further treatment is
recommended.
ARE ANY FURTHER TESTS NECESSARY?
The symptoms that hemorrhoids can cause can also occur with other abnormalities of the rectum or
anus. It is therefore important that a thorough examination is carried out and that the anus, anal
canal, and the beginning of the rectum are examined. If necessary, other additional tests should also
be carried out (extensive visual examination and/or X-ray of the colon). This is particularly common in
patients over the age of 50. In younger patients, an examination of the anus and anal canal is
generally sufficient. The doctor will perform the examination in a position that is uncomfortable for
the patient, namely the knee/elbow position or left lateral position. He will examine the area around
the anus and the anus itself and will also perform an internal examination of the anus and the
beginning of the rectum with his finger. A viewing tube will also be inserted into the anus to examine
the anal canal and the last part of the rectum. This will allow the doctor to determine whether there
are any hemorrhoids or other abnormalities.
If pain makes the examination impossible, it can be performed under local or general anesthesia. Your
treating physician will discuss with you which examinations are necessary before proceeding with
treatment. You will then be informed whether hemorrhoids have been diagnosed, whether treatment
is necessary, and if so, what kind.
WHAT ARE THE TREATMENT OPTIONS?
A logical treatment is to return the swollen tissue to its original position. This will remedy the
prolapse and the hemorrhoids will no longer cause any symptoms. A method that is widely used
nowadays is to tie off the excess mucous membrane using rubber bands (rubber band ligation). The
mucous membrane dies off within seven to ten days and the wound heals with a small scar. The
rubber band is later expelled naturally with the stool.
Another option is to inject an irritating liquid under the mucous membrane. The resulting reaction
causes the mucous membrane to stick to the underlying layer. A third treatment option also fixes the
mucous membrane to the underlying layer. This involves using infrared light to burn the mucous
membrane.
Combinations of the above treatments can also be performed. All procedures can be performed on
an outpatient basis in 15-30 minutes. In most cases, more than half of patients can expect good
results after the first outpatient treatment for hemorrhoids. If the prolapse of the hemorrhoids is
more severe, a second or third outpatient treatment may be necessary.
Surgery with hospital admission is rarely necessary for hemorrhoids. Surgical removal of hemorrhoids
is only performed in exceptional cases, when the hemorrhoids are very large and painful.
In cases of completely prolapsed and severely pinched hemorrhoids, which cause a lot of pain,
outpatient treatment is not possible. Surgery is then performed to relieve the tension in part of the
sphincter muscle. Due to the pain involved, this operation is usually performed under general
anesthesia.
Large hemorrhoids are surgically removed. Sometimes an internal bandage is applied for 24 hours.
POSSIBLE COMPLICATIONS OF SURGICAL TREATMENT
No procedure is free from the risk of complications. Surgery for hemorrhoids also carries the normal
risks of complications associated with surgery. These can be minor, such as inflammation of the vessel
where the IV is inserted, or a urinary tract infection. More troublesome is when post-operative
bleeding occurs. Sometimes an additional suture is placed in the ward; you may be taken back to the
operating room to be examined again under anesthesia. If you are taking blood-thinning medication,
you must inform your doctor before treatment. These medications increase the risk of post-operative
bleeding and will therefore need to be temporarily discontinued in consultation with your doctor.
When a rubber band leaves the rectum (the scab comes off the wound), some blood loss may occur.
If the blood loss seems to be more than a cupful, you should contact the hospital. Sometimes
immediate treatment via the hospital's Emergency Room/First Aid department is necessary.
Inflammation at the treatment site may cause a slight increase in temperature for a short period of
time.
The burns caused by the infrared treatment may cause some fluid secretion for a few days.
Cutting part of the sphincter muscle has little effect on the retention of stool. The treatment almost
never causes complications and the pain will usually decrease. The treatment can reduce the
unconscious control of flatulence and/or diarrhea.
In the now rarely necessary operations to remove hemorrhoids, the surgical area can be very painful
in the first few days after the operation. Painkillers will be prescribed for this.
A troublesome problem is passing stool after the operation. This can be painful and bloody the first
time, but once the stool has become softer due to the laxatives, it will become easier and the wounds
will heal more quickly. You will, of course, be given painkillers when necessary.
AFTER THE TREATMENT
No anesthesia or sedation is required for outpatient treatment. However, treatment with rubber
bands, injections, or infrared burns ( ) may cause discomfort for one to two days. The severity of the
symptoms may depend on the size of the treated area. Most patients do not need painkillers. A warm
bath or shower can reduce the symptoms. To prevent hard stools and straining, it is important to eat
extra fiber after the treatment.
After surgical treatment in the hospital, the wound must be cared for regularly. If you are unable to
do this yourself, the district nurse will be notified of your discharge in consultation with you. The
district nurse will contact you to make further arrangements. You will also need to use laxatives at
home for fourteen days. You will receive a prescription for this from the hospital.
If you are prescribed sitz baths in the hospital, you must continue with these at home. After
approximately fourteen days, when the wound is completely dry, you may stop the sitz baths. The
district nurse can also offer you help with this if necessary.
If you are experiencing difficulty with bowel movements, be sure to eat foods that are high in fiber.
Approximately one to three weeks after the operation, you will return to the outpatient clinic for a
checkup. Depending on your symptoms at that time, you may be asked to return to the outpatient
clinic a few more times.
The anal canal usually heals within three to four weeks after outpatient treatment. Patients usually
do not notice much. Normal daily activities can be resumed after one or two days.
After admission and treatment under anesthesia, you should expect to be off work for a longer period
of time.
Even though the hemorrhoids have been returned to their normal position after treatment,
symptoms may recur after several years. You can try to prevent this by following the above measures
and lifestyle rules as much as possible. This means eating more plant-based fiber, drinking plenty of
water, and avoiding straining.
If you still have questions after reading this brochure, please feel free to ask a nurse or your treating
physician.
|